|
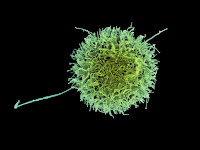
Mestastatic melanoma cells
|
Tracking the major cancer meetings has kept me occupied throughout October
and into November but left me with plenty of material for this, and future, blog
articles. A presentation at the UK’s NCRI conference on the increasing
mortality rate from melanoma in men (but not women, where mortality rates are generally
declining or stabilising), while alarming, did remind me of just how far
melanoma treatment has advanced in a few short years.
Prior to the availability of anti-CLTA-4 and anti-PD-1 immune
checkpoint inhibitors, overall survival from metastatic melanoma in developed
countries was around 25% after three years: combination immune checkpoint
inhibitor treatment has stretched this to over 60%, and use following surgery (“adjuvant”
use) significantly improves recurrence free survival.
Despite these successes, a significant need remains for alternative
treatments for those who fail, or are intolerant of, current immune inhibitor
checkpoint regimens and a gamut of investigational immunotherapies including
“personalized” or “individualised” peptide and mRNA therapeutic vaccines, cell
therapies and oncolytic virus therapies are in active clinical development.
That the immune system recognises melanoma as being “not self” has been
known for decades and means of usefully exploiting this distinction long
precede the discovery of immune checkpoints. Attempts to effectively boost the
anti-melanoma immune response through injection of the Bacille Calmette–Guérin
(BCG) tuberculosis vaccine were made in the 1970s, with mixed success. The
potent immunomodulators, interferon alpha (IFNα) and interleukin 2 (IL-2), were
approved for use in melanoma in the 1990s and still have a role in the treatment
of metastatic disease and adjuvant therapy.
Melanoma has long been an attractive target for cancer vaccine
development. A variety of melanoma antigens common to a majority of tumours -
“tumour-associated antigens” (TAAs), including gp100, GM2; tryosinase, MART-1
and MAGE-A3, have been exploited, either alone or in combination, in cell-based
and peptide therapeutic vaccines.
Cell-based vaccines (as either intact or processed tumour cells or as
cell-free lysates) offer the advantage of presenting a spectrum of TAAs,
although neither patient-derived (autologous) nor cultured tumour cell-derived
(allogeneic) cell-based melanoma vaccines, such as Melacine® (GSK/Schering) and
Canvaxin® (CancerVax/Serono), have made it through pivotal studies. M-VAX
(AVAX), a chemically-modified autologous cell vaccine, has been in late-stage
development limbo for over a decade.
Historically, peptide vaccines have fared no better, with a pivotal
study of Oncophage® (Antigenics), the manufacture of which involved isolation
of heat shock protein-peptide complexes from autologous tumour cells, being
abandoned, and a Phase III study of a MAGE-A3 peptide vaccine (GSK) being
terminated due to lack of obvious efficacy over placebo.
Adoptive cell transfer (ACT) involves the collection, isolation, ex
vivo expansion and (re)-infusion of autologous tumour-associated cytotoxic
T-cells. ACT using tumour-infiltrating lymphocytes (TIL) has occasionally attained
response rates of 40%-50% and complete remission in 10% to 25% of patients with
extensive metastatic disease: however, the complexity of ACT has essentially
confined it to clinical studies and compassionate use.
As is the case with other cancer indications, decades of disappointment
and inconsistency have not curbed the academic and commercial pursuit of
effective melanoma immunotherapies. Applying recent advances in technology-
next generation sequencing; gene transfer and editing; nucleic acid delivery-
to melanoma vaccine and cell therapy development might just make these old dogs
capable of new tricks.
Cancer vaccine efficacy is blunted by the immunosuppressive tumour
microenvironment: combination with immune checkpoint inhibitors is an obvious
means of increasing the odds of success and a number of studies combining
therapeutic vaccines with anti-PD-1 or anti-CTLA-4 immune checkpoint inhibitors
are underway. These agents may eventually be joined or replaced, by one or more
of the “next wave” of immune-oncology drugs directed at LAG3, CSF1-R, GITR or
at targets in the innate immune systems which can fire up the immune response.
Imlygic® (T-VEC: Amgen), an oncolytic virus therapy is“vaccine-like” in
effect, activating both the innate immune system and revealing hidden tumour
antigens (“neoantigens”) to the adaptive immune system through tumour lysis.
Combination with ipilimumab has shown improvement in response rates over
Imlygic® alone, and a Phase III combination study with pembrolizumab
(KEYNOTE-034) is ongoing. Early-stage studies of CAVATAK®, an investigational
virotherapy acquired by Merck & Co from Viralytics earlier this year, has
shown promise when combined with either pembrolizumab or ipilimumab.
The application of next generation sequencing technology and
bioinformatics could offer a practical route to bespoke melanoma vaccines, with
antigen selection and vaccine composition being determined by tumour and
patient genetic makeup. Neon Therapeutics is currently trialling a synthetic
peptide vaccine (NEO-PV-01) using sequencing of tumour biopsy material to
formulate a selection of up to 20 peptide-mimicking patient-specific
neoantigens. NantBioScience is pursuing a similar personalization strategy,
with expression of patient-specific neoantigens in yeast cells (YE-NEO-001).
The in vivo expression of
melanoma (and other cancer antigens) through the introduction of the
corresponding mRNA sequence is receiving increasing attention. Lipid complex
mRNA vaccines, encoding multiple melanoma TAAs or a personalised selection of
antigens, are now in early clinical studies (Lipo-MERIT and RO7198457:
BioNTech).
mRNA has brought a new twist to dendritic cell (DC) vaccination, where
DCs isolated from the patient are loaded with melanoma antigens to optimise
their processing and efficiency of presentation to the immune system. eTheRNA’s
TriMix technology combines mRNA encoding melanoma antigens with mRNA encoding
proteins known to enhance DC activation and maturation and to promote both
helper and cytotoxic T cell production. Durable clinical responses have been
achieved in melanoma patients who had failed previous treatments when the
TriMix-DC-MEL vaccine was administered in combination with ipilimumab.
Gene transfer may open up additional ACT strategies for melanoma.
T-cell receptor (TCR) gene transfer allows the generation of antigen-specific
lymphocytes from patient T-cells Early studies with melanoma antigen-specific
TCRs have shown modest response rates, although several have been marred by
severe adverse events due to the “off-target” destruction of normal
melanocytes.
The utility of ACT may be significantly improved through chimeric
antigen receptor (CAR-T) technology, where T-cell antigen receptors are
engineered to combine binding, signalling and co-stimulatory domains. Pilot
CAR-T studies are underway. Improvements in TIL ACT may be possible by using
CRISPR-CAS9 gene editing to increase the ability of T-cells to home in on
tumours.
Next generation cell therapies, including DC vaccination, are likely to
benefit from the broader expanding commercial interest in CAR-T and TCR
therapies which will likely lead to further improvements in manufacture and
assist in establishing the logistics necessary to delivery patient-specific
treatments. Growing use of semi- or wholly-automated cell product processing
will ultimately reduce costs and make the treatment of larger number of
patients viable.
Effective melanoma immunotherapy had been a long time in coming, but as
immune checkpoint inhibitor therapy has shown, revolution is possible.
Experimental melanoma immunotherapies still have a lot to prove, but with the
aid of across the board advances in immuno-oncology and other disciplines, we
may finally see vaccine and cell-based approaches becoming practical and
valuable treatment options.
Photo credit: Valencia, JC. NCI Center for Cancer Research