 |
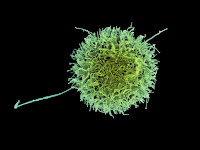
| Human natural killer (NK) cell. Add CAR for extra killing. |
Cancer immunotherapy, although far from offering universal cure, continues to rack up some remarkable successes. Immune checkpoint inhibitor treatment has transformed expectation in metastatic melanoma, non-small cell lung cancer and other advanced solid tumours, with new agents and novel combination therapies likely to further improve outcomes.
Cell-based
therapies in which patient T cells are genetically engineered to express a
protein construct (“chimeric antigen receptor”, hence CAR-T) specific for a
target cancer antigen, then expanded and infused to bring about tumour
destruction and long-term anti-tumour immunity. CAR-T treatment has achieved
unprecedented complete response rates in certain types of otherwise untreatable
childhood and adult leukaemia, although not without the risk of life-threatening
adverse events resulting from cytokine release and relapse through the escape
of cancer cells that do not express the selected target antigen.
Clinical
experience with CAR-T therapies is limited and so far confined to
haematological cancers (Kymriah® developed by Novartis and Yescarta®, developed
by Kite Pharma and since aquired by Gilead, only received FDA approval in August 2017 and October 2017,
respectively), but the potential of cell-based cancer treatment is such that substantial industrial and
academic effort is focused on development of next generation therapies capable
of tackling solid tumours, and which do not require complex and expensive patient-specific product
manufacture.
T cells are
not the only components of the immune system capable of tumour recognition and
destruction. So-called “natural killer” (NK cells- there’s a clue to their
purpose in the name) are part of the innate immune system, a first-line defence
that does not require the recognition and processing of foreign antigens to
function. NK cells possess a variety of tumour-recognising receptors with interaction
resulting in cancer cell destruction and upregulation of innate and adaptive
immune systems.
In contrast to
donated T cells (even when matched by tissue type), donated NK cells are not
identified as foreign, opening up the possibility of off-the-shelf (“allogeneic”)
treatments. NK cells are readily isolated from cord or peripheral blood and can
be maintained as a cell line. Human stem cell-derived NK cells might one day
prove suitable for industrial scale production. Moreover, as with T cells, NK
cells are amenable to transformation by viral vectors encoding chimeric antigen
receptor DNA.
A number of CAR-NK
clinical studies are underway, utilising NK cells from donors or cell lines
modified to express different cancer antigen receptors specific for lymphoma
and various forms of leukaemia; glioblastoma; non-small cell lung cancer, and
other solid tumours. Notably, several of these studies are sponsored by Chinese
clinical investigators and biopharma companies, echoing the country’s
substantial efforts in CAR-T product development.
CAR-NK product
development is not without problems, such as the efficiency of cell production
and need to optimise CAR design to minimise toxicity through “off target”
effects and to improve the specificity of intracellular signalling which kicks
NK cells into fighting mode. It’s too early to determine which of the available
sources of NK cells, if any, will result in superior outcomes. NK cells are
relatively short-lived and products based on a subset of longer-lived NK cells
may be required to induce lasting anti-tumour effects.
However, as
regulatory and clinical acceptance of CAR-T cell products demonstrates, the
complexities of cell-based therapy can be mastered: CAR-NK products will undoubtedly
benefit from this expanding knowledge base and through entering an environment with
growing payer acceptance of high-ticket cancer treatments.
Photo credit:
NIAID
